What it is not
- It does not mean you will not have a heart attack from surgery
- It does not mean you are free of heart disease
- It does not mean you won’t have heart problems as a result of surgery
- It is not an evaluation by your family practice doctor
What it consists of
A history and physical by a cardiologist (not your family doctor) and an EKG.
They may choose to have another examination to further investigate how your heart works – such as a cardiac CAT scan, a stress test, a nuclear stress test, an angiogram of the heart, an echo (ultrasound) of the heart. This is at the discretion of the cardiologist and is based upon your medical history,
Why do we want a cardiologist to see you?
Because even the most benign surgery is a stress test on your heart.
In surgery we want to know if there is something about your heart that needs us to treat your body in a certain way. We prepare for the worst in surgery. We anticipate in surgery that there will be “fluid shifts” that there will be blood loss. While our statistics tell us that the risks of bleeds requiring transfusions is small, we still want to know if there is something we need to do should in the event of blood loss, or just from the hyper coagulability of surgery (meaning, surgery makes people clot more).
For example: if you have an enlarged and thick heart the cardiologist will tell the surgeon and the anesthesiologist to not use as much fluid (meaning, keeping patients a bit on the “dry ” side or hypovolemic).
On the other hand if you have a stenotic aortic valve the cardiologist will tell the anesthesiologist and the surgeon to keep the patients on the “full” side, or have a lot of fluid on board.
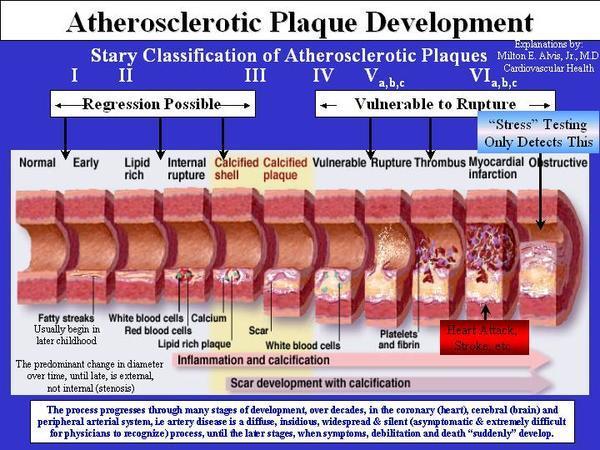
Heart attacks come after a build up of plaque on the vessels of the arteries leading to the heart. If these become blocked then there is no blood to the heart and you can die. You can see that a stress test – be it a nuclear stress test or a walking one, will show problems when there is a lot of plaque built up
Knowing how to manage a patient with heart disease, or certain heart conditions in advance allows us to decrease the risk of heart failure.
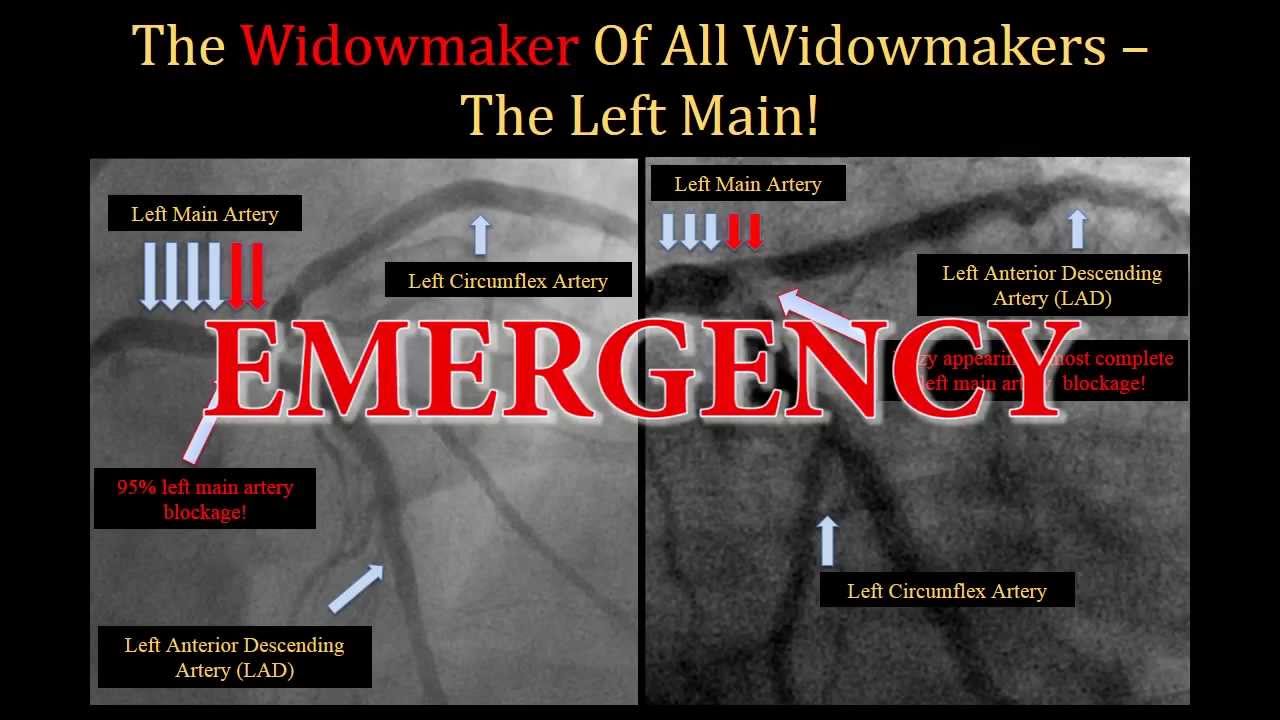
The widowmaker is a heart attack that happens when the left main artery is blocked. It is the most deadly heart attack with few people ever surviving.
My father-in-law, George, had a widow-maker lesion that was picked up on a stress test. George was scheduled to have a colonoscopy, but they would not even allow him to have the colonoscopy until the widow-maker was taken care of. When the cardiologist saw the films he admitted my George that day and did the stent. George was out the next day, and walking three to five miles after that. The cardiologist says he was lucky that they found it.

This is a thickened muscle of the heart. In this case caused by a bad heart valve. When hearts get so thick there is a risk of sudden cardiac death. This heart is about 600 grams – you can see a normal heart on the right. Few people survive such thick hearts for long. If the underlying cause is found and dealt with they can do ok, but many need heart transplants to survive.
Thickened heart muscle can come from a variety of reasons. This is the most common cause of sudden cardiac death among obese people. Often because of their arms having excess skin they have blood pressures that read “normal” when they are fairly “high.” High blood pressure leads to the heart needing to pump against more and more tissue. As people become obese they have more blood volume (every pound of fat has a mile of blood vessels) and it takes the heart more work to pump against that. Between under-reading blood pressure and the increase volume many obese patients are at risk for “hypertrophy” of the heart muscle. When obese people suddenly die, the most common cause is from the heart, and often from having hypertrophy of the heart.
If this is found we don’t do surgery. The heart has to be carefully treated with blood pressure medications (called after-load reducers) and the look for other causes – like bad heart valves. Sometimes the hypertrophy is so much — as in this case – that the only reasonable way to save their lives would be a heart transplant.
The most common cause of death after any surgery is from the heart.
For the vast majority of people, the heart is in good shape and should withstand surgery even with unanticipated blood loss.
But every year we find people who have heart disease that they didn’t know about. At least once a year we send someone to have their heart bypassed, or have a stent placed in their heart, or get a pacemaker, or some other intervention.
So when we ask you to see a cardiologist, know that most of the time you will be fine, and that will be a relief. But if they find something, we can treat it. And if we can treat it ahead of time it reduces the risk of death or permanent heart injury.
Who will we ask to see a cardiologist before surgery?
- Anyone who has heart disease (history of angioplasty, stents, bypass, heart disease).
- Anyone who has had long standing hypertension or high cholesterol levels.
- Anyone over the age of 50 (this is my rule, not a standard by any means).
Even with the best cardiologist, and with the easiest of surgery – a person can still develop cardiac problems and even die after a surgery. Surgery itself causes blood to clot easier. We depend on that in surgery, we depend on your body’s ability to clot. Your blood, after surgery, becomes “thicker” and people who have underlying heart disease can get a clot in their arteries going to their heart and this can be fatal.
What can you do? Surgery is a partnership with the patient. If you are on medication or given new medication by the cardiologist, please don’t stop it. Stopping some drugs without the anesthesiologist knowing or the surgeon knowing can lead to fatal consequences. If you are taking supplements, please list them all for your surgeon and your anesthesiologist as well as the cardiologist who is seeing you. Some of those drugs have profound influence on your heart – and most should be stopped long before going to surgery. If you develop severe chest pain after surgery, call 911.
