Leaky Gut: Facts and Fads
The latest fad of supplement makers is to talk about “gut health.” The latest boogyman for the gut is the “leaky gut.” The other name for leaky gut is intestinal permeability.
A Surgeon’s View
As a surgeon, a “leaky gut” is a devastating surgical emergency. Surgeons emergently operate to remove the gut that no longer has a barrier function.
The dark gut is dead and needs to be surgically removed. This gut has no barrier function and will allow bacteria from the inside of the small bowel to easily enter the patient’s bloodstream. Leading to septic shock and death.
The Non-Surgical Emergency or Chronic Leaky Gut
 But a leaky gut doesn’t have to be so dramatic. Not leading to septic shock or needing to be removed. In this model, the intestinal barrier is “leaky,” not to the point of causing sepsis. But the leaky gut enables small molecules to leak out of the gut into the bloodstream. Thus producing chronic inflammation.
But a leaky gut doesn’t have to be so dramatic. Not leading to septic shock or needing to be removed. In this model, the intestinal barrier is “leaky,” not to the point of causing sepsis. But the leaky gut enables small molecules to leak out of the gut into the bloodstream. Thus producing chronic inflammation.
Chronic inflammation may cause obesity. Emphasis on “may.”
Emulsifiers and Obesity

Emulsifiers disrupt the gut. Mice fed an identical amount of kibble develop obesity, while those without the emulsifiers have a normal weight.
Rodent studies have provided fascinating insights. Certain emulsifiers, when added to the diet of mice or rats, lead to obesity. In one experiment, rodents were fed identical amounts of kibble. But one group, emulsifiers, was added to their water. These emulsifiers, like polysorbate 80, not only produced obesity but also disrupted the microbiome of the gut (ref). But mice are not men.
When dietary emulsifiers are examined in humans, high levels cause disruption of the gut. However, there is little evidence that small amounts found in the food supply cause issues. (ref 4)
Non-Humans and Leaky Gut
While animal models are interesting, human studies provide useful information. That a rat or mouse has a leaky gut based on some intervention is not an equivalence in humans.
Functional Medicine and Leaky Gut
If you searched “leaky gut,” you will find a host of “functional medicine” doctors providing supplements, bone broth, probiotics, and other scams. On the shelves of drug stores and “health food stores,” you will find abundant supplements to “support gut health.”
Disease States and Leaky Gut
Functional medicine physicians associate many disease states with leaky gut. The following have little or no good evidence to be caused by a leaky gut:
- Alcoholic cirrhosis
- Asthma
- Autism
- Chronic fatigue syndrome
- Depression
- Eczema
- Environmental enteropathy
- Eosinophilic esophagitis
- Fibromyalgia
- Kwashiorkor
- Metabolic syndrome
- Multiple sclerosis
- Non-alcoholic fatty liver disease (NAFLD)
- Obesity
- Pancreatitis
- Parkinson’s disease
- Psoriasis
- Rheumatoid arthritis
Non-Controversial Causes of Leaky Gut
There is no doubt celiac disease, Crohn’s disease, radiation, and ulcers from non-steroidal anti-inflammatory drugs; certain bacteria can cause a change in intestinal permeability (another name for leaky gut). Celiac disease and Crohn’s disease have been studied for years (ref 2, ref 3). While we know gluten exacerbates the auto-immune function of those with Celiac disease, we do not yet have a mechanism for Crohn’s disease.
Gut Barrier Anatomy and Function
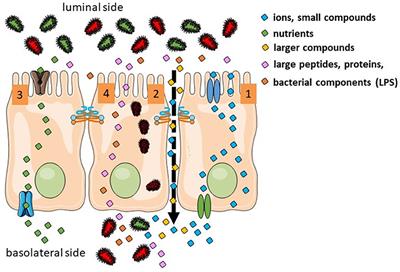
The small bowel’s purpose is primarily for the absorption of nutrients. Some nutrients are actively transported from the gut to the bloodstream, and some are passively absorbed. The gut must also serve as a barrier to prevent bacteria, toxins, and other materials from entering the body.
The first line of defense is the mucus layer of the gut. Secreted by Goblet cells, mucus prevents bacteria, toxins, and potential antigens from contact with the epithelial cells. There are multiple mucus proteins secreted. Gut immune cells secrete IgA antibodies into the mucus as a further defense against invaders.
Most research focuses on the tight junctions between intestinal epithelial cells.
Correlation or Causation
What if altered permeability is an association and not causation? While stress, antigens, and intense physical activity alter barrier function, there is no evidence it causes a clinical consequence. Finally, there is no evidence that barrier function leads to any disease. Nor is there any evidence that intervention to improve barrier function alters the natural history of disease (ref 4).
Mediterranean Diet and Barrier Function
In a recent clinical study, 260 women with the BRCA gene were assigned to the Mediterranean Diet or a control group (ref 5). These women were part of a study examining the effect of the Mediterranean diet and physical activity, who were at high risk for breast and ovarian cancer.
In the Mediterranean Diet group, there was an increase in short-chain fatty acids and fiber found in the stools. There was no statistically significant change in the plasma LBP or fecal zonulin. But in multiple-level regression, the change in short-change fatty acids did lead to a decrease in the permeability makers. When looking at the food groups, they found that vegetables, fruit, legumes, nuts, olives, wine, and total fiber were correlated with the shift in short-chain fatty acids and the shift in permeability makers.
The Mediterranean diet is fiber-rich, producing an increase in bacteria that produce short-chain fatty acids. The short-chain fatty acids appear to alter barrier function in this group of women.
Conclusions
While leaky gut is real, the significance is unknown. At the extremes, as surgeons see, it is deadly. In patients with ulcers or celiac disease, or Crohn’s disease – it is real. Yes, things can leak from the gut, but what can be done?
Turns out, maybe the Mediterranean Diet is the answer.
One this is certain – people will sell you all sorts of things –
Eat better, drink wine.