Apolipoprotein B (apoB) is the causative agent in atherosclerosis. If your apoB is low, you will not develop atherosclerosis. However, if your apoB is high, you could die young.
We know this because of genetic studies of people with different levels of apoB and their health outcomes.
What is Atherosclerosis of the heart?
Atherosclerosis is a progressive laying down of “plaque” in the wall of the coronary arteries. Since the coronary arteries feed the heart, this can lead to three outcomes:
- The plaque impinges on the artery. Thus, the plaque will decrease blood flow to the heart. This can lead to angina, or a poorly working cardiac muscle.
- The plaque can rupture (burst) into the artery. Next the body repairs this by clotting the blood. Thus, the blood flows to that portion of the heart is stopped. Without blood flow, the heart muscle starves, and if the flow isn’t restored, that part of the heart will die. This is a heart attack or myocardial infarction.
- The plaque can have no result. Meaning, it isn’t stopping blood flow to lead to angina, and it doesn’t occlude the artery.
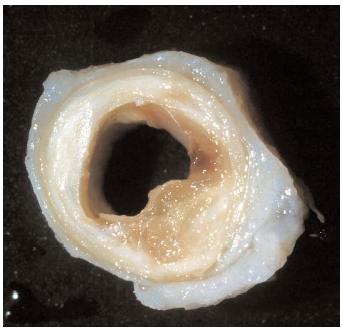
What is in the plaque?
In the above artery, you can see the yellow cholesterol in the wall. This is a “soft” plaque, like porridge.
The plaque is not inside the vessel. The artery is lined by a layer called the intima. So how does cholesterol get from the inside of the blood vessel to behind the layer?
The Process of Atherosclerotic Plaque Formation
Lipoprotein Entry into the Arterial Wall: The process begins when ApoB-containing lipoproteins pass through the endothelial layer of arteries. Normally, this layer acts as a barrier, but factors like high blood pressure or inflammation can make it more permeable, allowing these particles to accumulate beneath the endothelial cells.
Retention and Modification: Once inside the arterial wall, ApoB lipoproteins are trapped by proteoglycans (components of the extracellular matrix). These retained lipoproteins undergo modifications, such as oxidation, which makes them more likely to trigger inflammatory responses.
Inflammatory Response: The modified lipoproteins activate endothelial cells and attract immune cells like monocytes. These monocytes enter the arterial wall and transform into macrophages. Macrophages engulf the modified lipoproteins, turning into foam cells, which are a hallmark of early atherosclerotic plaque.
Plaque Development: Over time, foam cells accumulate, leading to the formation of fatty streaks in the arterial wall. Smooth muscle cells migrate into the intimal layer of the artery, contributing to the formation of a fibrous cap that covers the plaque. This cap consists of connective tissue, calcium, and cholesterol deposits.
Progression and Complications: As the plaque grows, it narrows the artery and restricts blood flow. If the fibrous cap ruptures, it can lead to the formation of a blood clot (thrombus), which may block the artery entirely, causing a heart attack or stroke.
Preventing Plaque Formation
Understanding how ApoB-containing lipoproteins contribute to atherosclerosis underscores the importance of managing blood cholesterol levels. Lifestyle changes such as diet, exercise, and medications like statins can reduce LDL levels, lowering the risk of plaque formation and subsequent cardiovascular events.
Atherosclerosis is a gradual process that starts with the seemingly harmless entry of ApoB lipoproteins into arterial walls. By addressing the risk factors that promote lipoprotein retention and inflammation, the progression of atherosclerosis can be slowed or prevented.
LDL particle size
LDL particles can vary in size, and it was previously believed smaller, denser LDL particles were more atherogenic than larger, buoyant ones. However, research has shown that the number of LDL particles, regardless of size, is a more significant determinant of cardiovascular risk. Studies indicate that the concentration of LDL particles is more closely associated with atherosclerosis than the size of the particles themselves.
The ApoB Factor: Why It’s a Big Deal
ApoB is a protein found on the surface of atherogenic lipoproteins, including LDL, VLDL, and IDL. Each of these particles contains one ApoB molecule, making ApoB a direct measure of the number of atherogenic particles in the blood. This measurement is crucial because it provides a clearer picture of the atherogenic burden in the bloodstream than LDL-C alone.
Why ApoB is the Star Player
Direct Measure of Risk: ApoB directly measures the number of atherogenic particles, providing a more accurate assessment of cardiovascular risk.
Independent of Particle Size: Unlike LDL size, which can vary and complicate risk assessment, ApoB consistently reflects the number of risk-contributing particles.
Predictive Power: Numerous studies have shown that ApoB is a better predictor of cardiovascular events than LDL-C or other traditional lipid measures.
ApoB: Direct Measurement of Atherogenic Particles
Apolipoprotein B (ApoB) is the main protein component of several lipoproteins, including low-density lipoprotein (LDL), very-low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and lipoprotein(a). Each atherogenic particle contains one molecule of ApoB, making ApoB a direct measure of the number of atherogenic particles circulating in the bloodstream.
Key Points:
Direct Indicator of Particle Number: Since each atherogenic lipoprotein particle has one ApoB molecule, measuring ApoB provides an accurate count of these particles. This is crucial, because the more atherogenic particles present, the higher the risk of these particles penetrating the arterial walls and contributing to plaque formation.
Independent of Cholesterol Content:
The cholesterol content does not influence ApoB measurement within these particles. Therefore, it provides a clearer picture of cardiovascular risk, especially in cases where LDL cholesterol (LDL-C) levels might be normal, but the number of LDL particles (and thus ApoB) is high.
HDL-TG Ratio: A Marker of Lipid Metabolism
The HDL-TG ratio, which is the ratio of high-density lipoprotein cholesterol (HDL-C) to triglycerides (TG), is used as a marker to assess lipid metabolism and insulin resistance. A high HDL-TG ratio generally indicates a favorable lipid profile and a lower risk of cardiovascular disease. However, this ratio has limitations:
Indirect vs direct measure:
Indirect Measurement: The HDL-TG ratio provides an indirect measure of cardiovascular risk. It does not directly quantify the number of atherogenic particles, but rather gives a sense of lipid metabolism status. While a low HDL-C and high TG level can indicate higher cardiovascular risk, it doesn’t directly account for the number of atherogenic particles present.
Variability and Confounding Factors:
Several factors can influence the ratio, including lifestyle, diet, and metabolic disorders, which can confound its predictive value for cardiovascular risk. Additionally, HDL-C levels alone have not consistently been shown to correlate with reduced cardiovascular risk, as HDL particles can vary in functionality.
Why ApoB is More Important
Predictive Power: Numerous studies have shown that ApoB is a stronger predictor of cardiovascular events than the HDL-TG ratio. For instance, the INTERHEART study highlighted that ApoB levels were more predictive of myocardial infarction than other lipid markers, including the HDL-TG ratio.
Comprehensive Risk Assessment: ApoB accounts for all atherogenic particles, providing a more comprehensive assessment of cardiovascular risk compared to measures that only consider cholesterol content or ratios of different lipid components.
Focusing on the Right Metric
In summary, the focus has shifted from LDL particle size to the number of atherogenic particles, as measured by ApoB. This shift is grounded in the understanding that cardiovascular disease risk is more closely linked to the number of these particles, rather than their size or cholesterol content alone. Therefore, ApoB provides a more accurate and reliable measure for assessing cardiovascular risk.
Conclusion
While both ApoB and the HDL-TG ratio can provide valuable information about lipid metabolism and cardiovascular risk, ApoB is considered more important due to its direct measurement of atherogenic particles. This makes it a more reliable and comprehensive marker for assessing the risk of atherosclerosis and related cardiovascular events.
Citations:
Sniderman, A. D., & Tsimikas, S. (2014). Apolipoprotein B. Circulation, 129(11), 1112-1120.
Packard, C. J., & Shepherd, J. (1999). Lipoprotein heterogeneity and apolipoprotein B metabolism. Atherosclerosis, 141(1), 27-42.
McQueen, M. J., Hawken, S., Wang, X., Ounpuu, S., Sniderman, A., Probstfield, J., … & Yusuf, S. (2008). Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. The Lancet, 372(9634), 224-233.
Cromwell, W. C., & Otvos, J. D. (2004). Low-density lipoprotein particle number and risk for cardiovascular disease. Current Atherosclerosis Reports, 6(5), 381-387.
Mora, S., Otvos, J. D., Rifai, N., Rosenson, R. S., Buring, J. E., & Ridker, P. M. (2009). Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation, 119(17), 931-939.
Packard, C. J., & Shepherd, J. (1999). Lipoprotein heterogeneity and apolipoprotein B metabolism. Atherosclerosis, 141(1), 27-42.
Sniderman, A. D., & Furberg, C. D. (2008). Age as a modifiable risk factor for cardiovascular disease. The Lancet, 371(9623), 1547-1548.
Cromwell, W. C., & Otvos, J. D. (2004). Low-density lipoprotein particle number and risk for cardiovascular disease. Current Atherosclerosis Reports, 6(5), 381-387.
Sniderman, A. D., & Tsimikas, S. (2014). Apolipoprotein B. Circulation, 129(11), 1112-1120.
Harchaoui, K. E., Visser, M. E., Kastelein, J. J., Stroes, E. S., & Dallinga-Thie, G. M. (2009). Triglycerides and cardiovascular risk. Current Cardiology Reviews, 5(3), 216-222.
McQueen, M. J., Hawken, S., Wang, X., Ounpuu, S., Sniderman, A., Probstfield, J., … & Yusuf, S. (2008). Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. The Lancet, 372(9634), 224-233.