The Cyclical Nature of Autoimmune Diseases: A Huckster’s Playground
Autoimmune diseases are notoriously difficult to manage because they don’t follow a linear progression. Patients often experience periods of remission, where symptoms lessen or disappear, followed by flare-ups, where symptoms return, sometimes worse than before. This cyclical nature gives the illusion that certain “treatments” or lifestyle changes are working when, in reality, the disease is simply following its natural course.
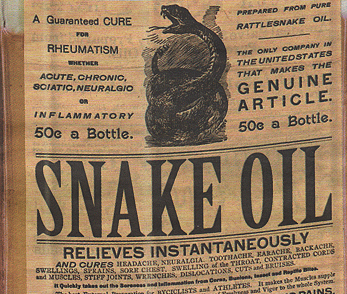
Hucksters exploit this ebb and flow, offering unproven solutions and claiming credit for any improvements that coincide with the natural remission phase. When symptoms return during a flare-up, they may shift the blame to the patient, suggesting they didn’t follow the regimen properly or need to try an even more restrictive approach.
In many cases, these alternative therapies center around the idea that gut issues cause autoimmune diseases, particularly leaky gut syndrome. The pitch is simple: repair the gut, and the immune system will stop attacking the body. Unfortunately, the science doesn’t back this up.
Why the Gut Isn’t the Root Cause of Autoimmune Disease
It’s true that there is a connection between the gut and the immune system. In fact, about 70% of the immune system resides in the gut, and gut bacteria (the microbiome) play a role in regulating immune responses. However, autoimmune diseases are far more complex than just a gut issue.
Genetic predispositions primarily drive Autoimmune diseases, environmental triggers, and immune system dysregulation. While diet and gut health can influence immune responses, there’s no evidence that simply “healing” the gut will reverse the course of autoimmune diseases. The immune system in these conditions has gone awry in ways that are not fully understood, and current medical treatments focus on suppressing overactive immune responses and managing symptoms—not on gut health alone.
Myasthenia Gravis (MG) is an autoimmune disease where medical treatment significantly outperforms dietary interventions.
MG is characterized by autoantibodies targeting the neuromuscular junction, leading to fluctuating muscle weakness and fatigability. The primary treatment modalities for MG involve immunosuppressive therapies and precision medicine approaches.
Current treatment guidelines, as discussed by Cavalcante et al., highlight the use of immunosuppressive therapies such as corticosteroids, azathioprine, and mycophenolate mofetil to control symptoms and improve muscle strength. (reference here)
Additionally, novel biological drugs targeting B cell activation, antibody recycling, and complement system-mediated neuromuscular junction damage have shown efficacy and safety in clinical trials. These precision medicine approaches are tailored to the patient’s specific immunopathogenic mechanisms, offering a more targeted and effective treatment strategy.
In contrast, dietary interventions have not demonstrated significant efficacy in managing MG. While general nutritional support is important for overall health, there is no specific diet that can modulate the autoimmune mechanisms underlying MG to the same extent as pharmacological treatments.
In summary, medicine does better than diet in managing Myasthenia Gravis, with immunosuppressive therapies and precision medicine approaches being the cornerstone of treatment.[1]
Here’s why relying on gut health as the sole solution is like using a garden hose to fight a forest fire:
A. The Complexity of Autoimmune Dysregulation
Autoimmune diseases involve dysregulation at multiple levels of the immune system. In diseases like lupus or multiple sclerosis, immune cells are mistaking the body’s own tissues for foreign invaders. This misidentification isn’t simply the result of a leaky gut; it’s a deeper issue with how the body’s T-cells, B-cells, and other immune components are functioning.
Medical treatments for autoimmune conditions, such as biologics and immunosuppressants, target these complex pathways to reduce inflammation and prevent further tissue damage. These therapies are carefully designed to modulate specific immune processes—something that diet and gut health alone can’t achieve.
B. Gut Health Cannot Reverse Severe Immune Attacks
Imagine trying to put out a raging forest fire with a garden hose—that’s what focusing solely on gut health is like when trying to manage autoimmune flare-ups. Autoimmune diseases can cause severe damage to the organs, such as the joints, kidneys, or central nervous system, depending on the condition. These diseases are often life-altering and, in severe cases, life-threatening.
Even if the gut plays some role in immune regulation, “fixing” the gut doesn’t address the immune attacks happening in vital organs throughout the body. Managing an autoimmune condition requires powerful treatments that target these immune responses at the source, not superficial changes to the digestive system.
C. Gut-Focused Diets Can Be Restrictive and Harmful
Another major issue with the gut-healing approach is that it often involves restrictive diets that cut out whole food groups in the name of reducing inflammation or healing the gut lining. These diets, such as the autoimmune protocol (AIP) or extreme versions of the paleo diet, are promoted as cures but lack strong scientific backing.
For many patients, these diets can lead to nutrient deficiencies, unnecessary food anxiety, and added stress—none of which is helpful when managing a chronic condition. Worse, some people may forego or delay important medical treatments, opting instead for these restrictive, gut-healing diets in hopes of a cure. This can lead to uncontrolled disease progression and irreversible damage to organs.
What We Do Know: The Gut’s Role in Autoimmune Disease Management
This isn’t to say the gut has no role in autoimmune disease—far from it. Gut health can influence overall health, including the immune system, and managing autoimmune diseases often includes dietary adjustments to improve symptom management. But diet should be seen as one tool in a larger toolbox, not the magic bullet.
For example:
Probiotics and prebiotics may support gut health and help modulate immune responses in some cases, though the evidence is still emerging.
However, if these patients are not appropriately followed, they can develop kidney involvement leading to loss of function or severe joint destruction for RA type, or even severe vasculitis, and none of these conditions are treated by or recognized by chiropractors