
Photo by David Shankbone
The medical details are incomplete- but she may have had a heart attack, leading to a cardiac arrest (the heart stopped) and in spite of being at a physicians office or outpatient center, she needed to be transported to a hospital for advanced care.
When the brain is without nutrients for a period of time there can be irreparable damage. By placing the brain into a coma (so it has little function) it allows the brain to heal. When they reversed these drugs to determine her neurologic status there were three distinct possibilities: she may wake up completely, she may have lost function, she may remain in a “vegetative” state – with minimal function. Initial results were that she had some “function.” Sadly, there was not enough, and she died.
We do not know if she underwent CPR, or not- although suspect she did as they state that she was in “full cardiac arrest.”
The prognosis for this situation is always poor. When people have underlying disease even if they are in hospitals with the best of care, they often do not recover from a cardiac arrest.
Incidence of Cardiac Arrest
Cardiac arrest during an outpatient procedure (like an endoscopy) is a rare and unexpected event. Surgeons and anesthesiologists spend a fair bit of time determining risk factors, and with some patients will ask cardiologists to see patients to “clear” them for the procedure. Even in the best clinical judgement, and under the best supervision patients with underlying cardiac disease can suddenly go into cardiac arrest.
Odds Are Poor
If you have a cardiac arrest in a hospital, where properly trained people administer up-to-date CPR and medications, the chance of survival is less than 25%, according to the American Heart Association. One fourth of all cardiac disease is discovered when patients die of the disease – sudden cardiac death, or full cardiac arrest.
The Unknown Risk
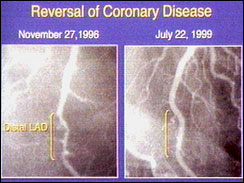
Cardiac arrest happens when either the arteries feeding the heart clog suddenly, depriving the heart of blood supply and lead to cardiac muscle death. The second form of cardiac arrest is when the electrical supply to the heart fails and the person suddenly dies. The second type of arrest typically does well in a hospital setting, as they need some electric shock to restart the heart, but the first type is far more devastating.
Tim Russert, the host of NBC’s ‘Meet the Press’ was under a cardiologist’s supervision, had known cardiac disease, was being treated for it, and yet died of a massive heart attack while exercising.
News reports are discussing that she “should not have had this procedure as an outpatient” and some are “looking for someone to blame,” manifest an unlikely outcome. These procedures are done by the thousands in outpatient centers, and had her procedure been done in a hospital the outcome likely would not change. This is a rare and unexpected, and tragic event that does happen.
How Can We Find Out
The problem with heart disease is that if there is disease in the artery it does not mean it would manifest itself with any of the common tests we do. For example: my father-in-law had the major artery of his heart 90 percent blocked, but passed the stress test and ultrasound of his heart. Only because the cardiologist did a CT angiogram of his heart did they discover the extent of his disease.
Often a heart attack can come, not from a significant blockage of the heart- but a partial blockage that’s not causing any issue. It might be 30% blocked – not enough to do a bypass or a stent – but it can cause a plug in the heart and erupt sudden cardiac death.
In spite of our best efforts, doctors cannot predict who might develop this rare condition. Chances are if it’s from underlying heart disease Joan Rivers would have had a major cardiac event in the next few weeks. The advantage of being at an outpatient center is that she was in a facility where they could perform CPR to give her a chance to survive.
May she rest in peace.
