Heart disease is the number one cause of death in the United States, with one in three people dying of heart disease. It is also the leading cause of illness.
Heart attacks can be prevented by certain drugs, called statins, and yet those drugs have some side effects, so they are not meant for everyone. So who should take them. Statins are a class of lipid-lowering medications that function by inhibiting the enzyme 3-hydroxy-3-methyl-glutaryl coenzyme A reductase, which is involved in the rate-limiting step in the production of cholesterol. Statins reduce levels of total cholesterol and LDL-C and, to a lesser extent, triglycerides, and probably have anti-inflammatory and plaque stabilization effects as well.
A list of statins available in the US is below
- atorvastatin (Lipitor),
- fluvastatin (Lescol, Lescol XL),
- lovastatin (Mevacor, Altoprev),
- pravastatin (Pravachol),
- rosuvastatin (Crestor),
- simvastatin (Zocor), and.
- pitavastatin (Livalo).
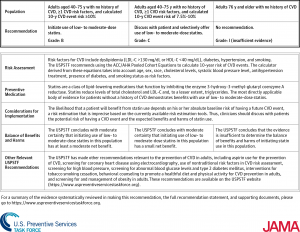
The latest recommendations from the United States Preventative Services Task Force (USPSTF) came out with the following:
If you have had a heart attack, then you should be on a statin drug.
If you are between the age of 40 and 75 and have a 10 per cent risk of having a heart attack in the next ten years then you should probably be on the drug. To determine the risk of having a heart attack there are various calculators out there. But those calculators often give a higher risk factor. Therefore it is felt that if you have a risk of at least 7.5 % you should begin a discussion with your doctor about being on statin therapy for a lifetime.
Risk factors include: diabetes, hypertension, age, gender, and cholesterol levels. Those all increase the risk of heart disease and require statins.
From JAMA:
The USPSTF found adequate evidence that the harms of low- to moderate-dose statin use in adults aged 40 to 75 years are small. Randomized clinical trials (RCTs) of statin use for the primary prevention of CVD events have largely used low and moderate doses; under these conditions, statin use was not associated with serious adverse events such as cancer, severely elevated liver enzyme levels, or severe muscle-related harms. However, evidence concerning the association between statin use and diabetes mellitus is mixed, with 1 prevention trial suggesting that there may be a small increased risk of developing diabetes with use of high-dose statins. Myalgia is a commonly reported adverse effect of statins, but placebo-controlled trial data do not support the conclusion that statin use has a major causative role in its occurrence. Evidence for cognitive harms is relatively sparse; further research would be needed to more definitively establish the relationship between statin use and cognitive function. The USPSTF found no clear evidence of decreased cognitive function associated with statin use. These findings are consistent with those from a recent systematic review of RCTs and observational studies assessing the effect of statins on cognition that found no effect on incidence of Alzheimer disease or dementia.7 The recently published HOPE-3 (Heart Outcomes Prevention Evaluation 3) trial found that statin use increased risk of cataract surgery, which was unanticipated and not a predetermined outcome of the trial.8 None of the other primary prevention trials reported this outcome.9
REFERENCE:
Click slide below for larger view