Decreasing cholesterol: drugs and diet
There is a persistent belief that lifestyle can take care of all cholesterol problems. Lifestyle can make things worse, but once things are worse, it cannot make things better.
Once you have disease, or cholesterol is higher, you need treatment often beyond lifestyle management.
This distresses many people, who wish to have control over their fate.
High cholesterol is one of the main causes of heart attacks, strokes, and peripheral vascular disease. You can lower cholesterol through diet and exercise by as much as 15 percent. Lifestyle changes are the first choice to decrease cholesterol. Modern drugs, however, will lower cholesterol levels far more than diet or exercise.
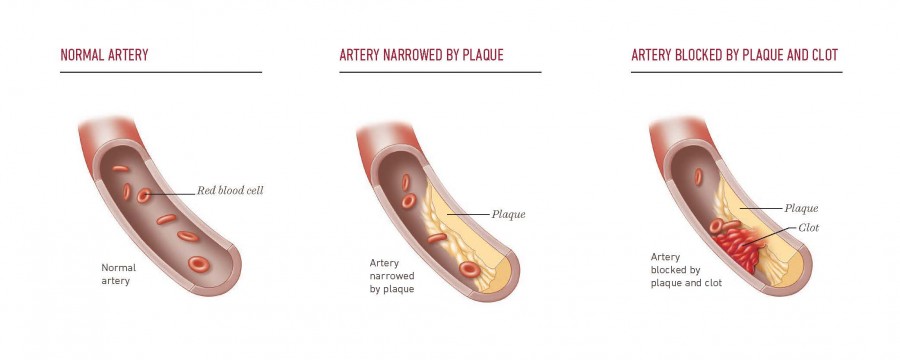
The progressive changes of a vessel
The normal artery, as shown below, is a free flowing blood vessel. When a person is in their late teens, there is already fatty formation on the inside of the vessel wall.
As more fat is deposited in the vessel wall, blood flow decreases, leading to ischemia in the end organ.
Angina, or heart pain, occurs when there is insufficient blood flow to the heart secondary to an artery narrowed by plaque.
Factors contributing to atherosclerotic plaque formation
Damage to the blood vessel begins the process of
- Smoking
- Hypertension
- High blood sugars
- Diets rich in saturated fats and refined grains
However, the lower the level of LDL, the less risk those factors become, as you shall see.
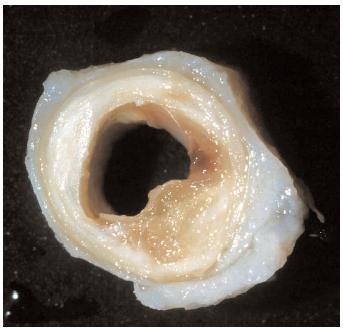
Anatomy of the Blood Vessel
If you examine the autopsy specimen of the coronary artery above, the blood flows through that lumen. The inner wall, the wall the blood comes into contact with, is called the endothelium. There are three layers to the wall of an artery:
- Tunica intima
- Tunica Media
- Tunica Adventicia
Atherosclerosis begins when the cholesterol transport protein enters the wall of the tunica media, whose first layer is the endothelium.
Discovery of LDL
In 1954, Dr. John Gofman reported the discovery of LDL and HDL. These were the particles found when he separated plasma cholesterol-carrying lipoproteins with an ultracentrifuge. Gofman was the first to note that heart attack patients had high LDL levels. The correlation of high LDL and heart attacks has been called “one of the most profound epidemiologic correlations in all of medicine.”
High LDL levels have been shown to correlate with atherosclerosis in all species studied.
High LDL and Atherosclerosis
The higher the LDL level, the faster atherosclerosis develops. Factors that increase atherosclerosis are those which injure blood vessels: smoking, hypertension, hyperglycemia, and genetic factors that predispose endothelium to early injury.
High LDL levels can lead to heart attacks in children as young as 6 years old. This rare form of homozygous familial hypercholesterolemia inspired Brown and Goldstein to elucidate the genetic defect in the receptor for LDL.
Discovery of the LDL receptor defect
Brown and Goldstein discovered that when LDL receptors are defective, it leads to the following:
- LDL particles circulate for a long time
- This leads to an increase in plasma levels of LDL
- As a result, more deposits are made into the arteries
- Creating atherosclerotic plaques
Lowering LDL by feedback
To keep blood LDL constant, your body uses a feedback mechanism. As your LDL levels increase, the target tissues produce more receptors to take up the LDL. If the LDL receptor is defective, the liver continues to increase production of LDL.
Brown and Goldstein speculated that an HMG CoA reductase inhibitor would deprive liver cells of endogenous synthesis as a source of cholesterol. This deprivation would relieve the feedback repression of LDL receptors, and the resultant increase in LDL receptors would lower plasma LDL.
Developing the first statins
The FDA approved the first statin 1987, Mevacor, which reduced plasma levels of LDL and was well tolerated. It was only theory that lowering LDL would reduce heart attacks.
Statins Reduce Heart Attacks and Prolong Life
Statins block cholesterol synthesis, which causes the cell to increase LDL receptors, which further decrease cholesterol in blood plasma.
The first study showing that statins not only reduce LDL, decrease heart attacks, and prolong life was reported in 1994. These studies have been repeated:
The 2002 study was large enough to show a reduction in relative risk even when subjects had risk factors such as diabetes, hypertension and smoking.
For each reduction of LDL cholesterol by 40 mg /dl cardiovascular events are reduced by 20%. This even applies to people considered low-risk (ref).
Better Genetics
In addition to people with high cholesterol, there are those with naturally low levels of cholesterol. These individuals live long lives with abnormally low levels of heart disease, even if they have other risk factors (ref). Yes, I want this mutation!
This genetic mutation led to a new class of drugs to decrease cholesterol, the PCSK9 class of drugs.
Lowering LDL over time is the key
Genetic studies, statin studies and PCSK9 studies show that lowering LDL longer leads to lower atherosclerotic disease.
People with PCSK9 mutations may never develop atherosclerotic plaque because they have low LDL levels throughout their lives.
In many statin studies, patients were treated only when they were at high risk of coronary disease, which means they had already established atherosclerosis. Once the disease is diagnosed, patients may need a much more severe LDL reduction to prevent an event.
Bringing it back to Ancel Keys
One of the cohorts that Ancel Keys studied was in a coastal village in Japan. The men in that village had a 90% reduction in their LDL. This lifelong reduction also led to a 90% reduction in their cardiac mortality. (ref) . The PCSk9 mutations also resulted in a 90% reduction in mortality from a similar reduction in LDL.
Inflammation and cholesterol
Lowering cholesterol reduces the risk of heart disease, independent of inflammation. While some blame inflammation alone as a cause of atherosclerosis, it is less a cause and more a result. Inflammation is important to repair tissues, but is not the cause of the trauma. Reducing LDL reduces the risk of heart disease.
Inflammation and oxidized cholesterol have been speculated as a cause of heart disease.
Red Meat
Red meat is nutritionally and calorie rich. But it is also rich in saturated fat. Saturated fat leads to high blood cholesterol. And high blood cholesterol leads to plaque in the arteries. One does not need to give up meat. But, limiting red meat to four ounces a day is protective.
Vegetables and other fiber rich foods provide an additional protective effect with the consumption of meat. It appears that the increase in soluble fiber, as well as phytoestrogens from the fiber, reduces the pathway of cholesterol absorption. In addition, they decrease the risk of colon cancer.
REFERENCES:
Brown MS, Goldstein JL. A receptor-mediated pathway for cholesterol homeostasis. Science. 1986 Apr 4;232(4746):34-47. doi: 10.1126/science.3513311. PMID: 3513311.
Brown MS, Goldstein JL. Cholesterol feedback: from Schoenheimer’s bottle to Scap’s MELADL. J Lipid Res. 2009 Apr;50 Suppl(Suppl):S15-27. doi: 10.1194/jlr.R800054-JLR200. Epub 2008 Oct 29. PMID: 18974038; PMCID: PMC2674699.
Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012 Aug 11;380(9841):581-90. doi: 10.1016/S0140-6736(12)60367-5. Epub 2012 May 17. PMID: 22607822; PMCID: PMC3437972.
Cohen JC, Boerwinkle E, Mosley TH Jr, Hobbs HH. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med. 2006 Mar 23;354(12):1264-72. doi: 10.1056/NEJMoa054013. PMID: 16554528.
Gofman JW, Delalla O, Glazier F, Freeman NK, Lindgren FT, Nichols AV, Strisower B, Tamplin AR. The serum lipoprotein transport system in health, metabolic disorders, atherosclerosis and coronary heart disease. J Clin Lipidol. 2007 May;1(2):104-41. doi: 10.1016/j.jacl.2007.03.001. PMID: 21291675.
GOFMAN JW, RUBIN L, McGINLEY JP, JONES HB. Hyperlipoproteinemia. Am J Med. 1954 Oct;17(4):514-20. doi: 10.1016/0002-9343(54)90126-6. PMID: 13197415.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002 Jul 6;360(9326):7-22. doi: 10.1016/S0140-6736(02)09327-3. PMID: 12114036.
Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998 Nov 5;339(19):1349-57. doi: 10.1056/NEJM199811053391902. PMID: 9841303.
Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994 Nov 19;344(8934):1383-9. PMID: 7968073.
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996 Oct 3;335(14):1001-9. doi: 10.1056/NEJM199610033351401. PMID: 8801446.
Storey BC, Staplin N, Haynes R, Reith C, Emberson J, Herrington WG, Wheeler DC, Walker R, Fellström B, Wanner C, Landray MJ, Baigent C; SHARP Collaborative Group. Lowering LDL cholesterol reduces cardiovascular risk independently of presence of inflammation. Kidney Int. 2018 Apr;93(4):1000-1007. doi: 10.1016/j.kint.2017.09.011. Epub 2017 Nov 14. PMID: 29146277; PMCID: PMC5978933.
Willett WC. Dietary fats and coronary heart disease. J Intern Med. 2012 Jul;272(1):13-24. doi: 10.1111/j.1365-2796.2012.02553.x. PMID: 22583051.
“1. Introduction”. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease, Cambridge, MA and London, England: Harvard University Press, 2013, pp. 1-16. https://doi.org/10.4159/harvard.9780674497887.intro